Why measure ‘Cholinesterase’?
Cholinesterase activity and phenotype studies in a patient can be used to predict the degree of potential post-operative paralysis following the use of the short reacting muscle relaxant suxamethonium or mivacurium.
It can also be used as a monitor of exposure to organic phosphorus compounds in the agricultural and chemical industries.
The laboratory measures the enzyme activity in the patient’s blood and also determines the biochemical phenotype, which is an indicator of the enzymes ability to break down the drug. Both factors are involved in determining that patient’s risk of paralysis. Low enzyme activity may be related to the phenotype, or can occur in a patient with a normal (Usual) phenotype if there are any secondary factors (see list below).
The phenotype tells you about the behaviour of the enzyme whereas a genotype tells you about the particular mutations that the patient has inherited. A phenotype can be made up of more than one genotype.
Who to measure ‘Cholinesterase’ in
Measurement of cholinesterase is indicated in anyone who has already experienced an apnoea in theatre, or in first degree relatives of patients who have been found to have an abnormality in enzyme activity or phenotype.
Sample collection
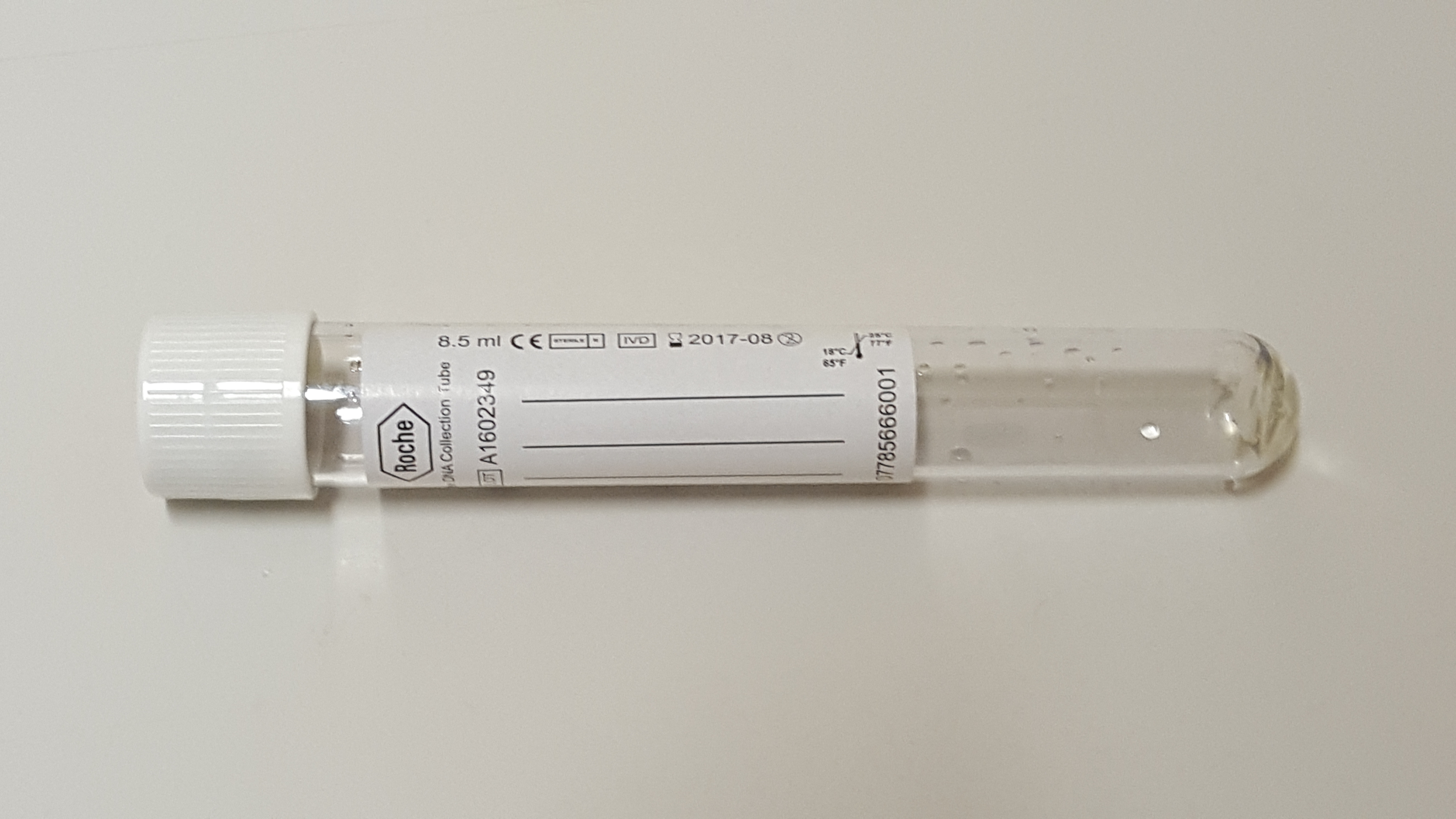
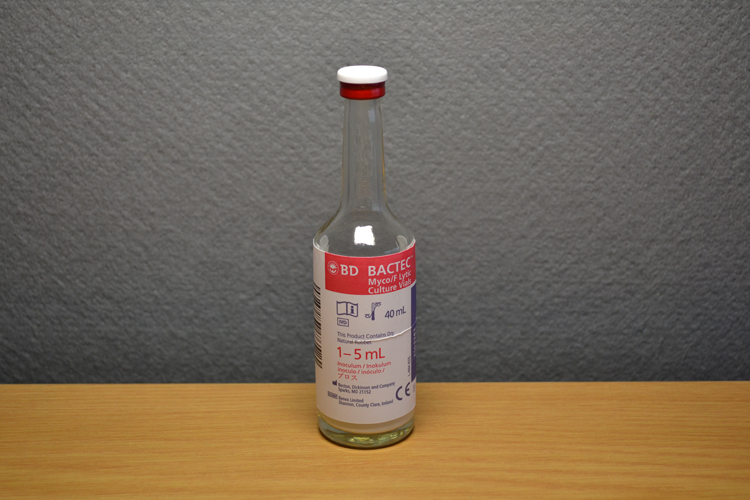
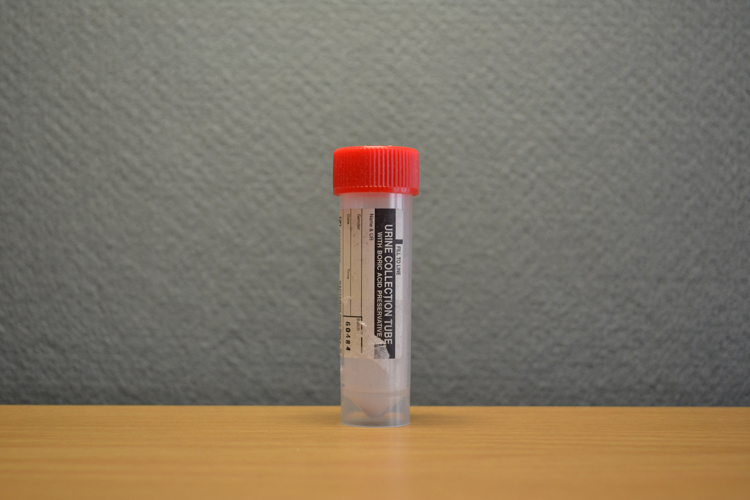
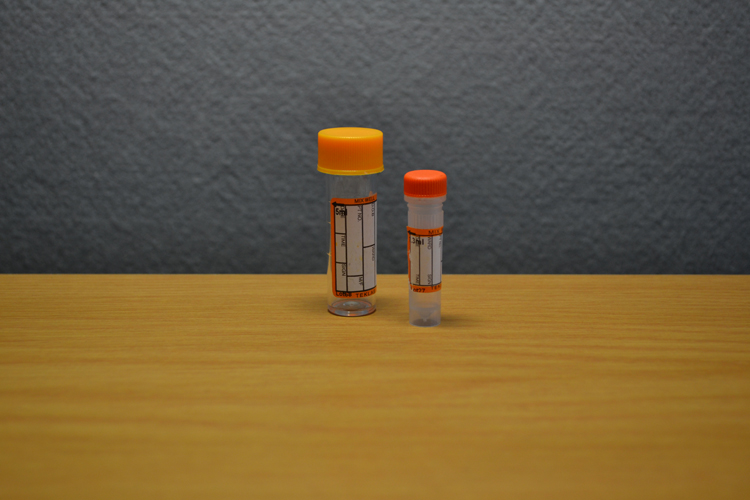
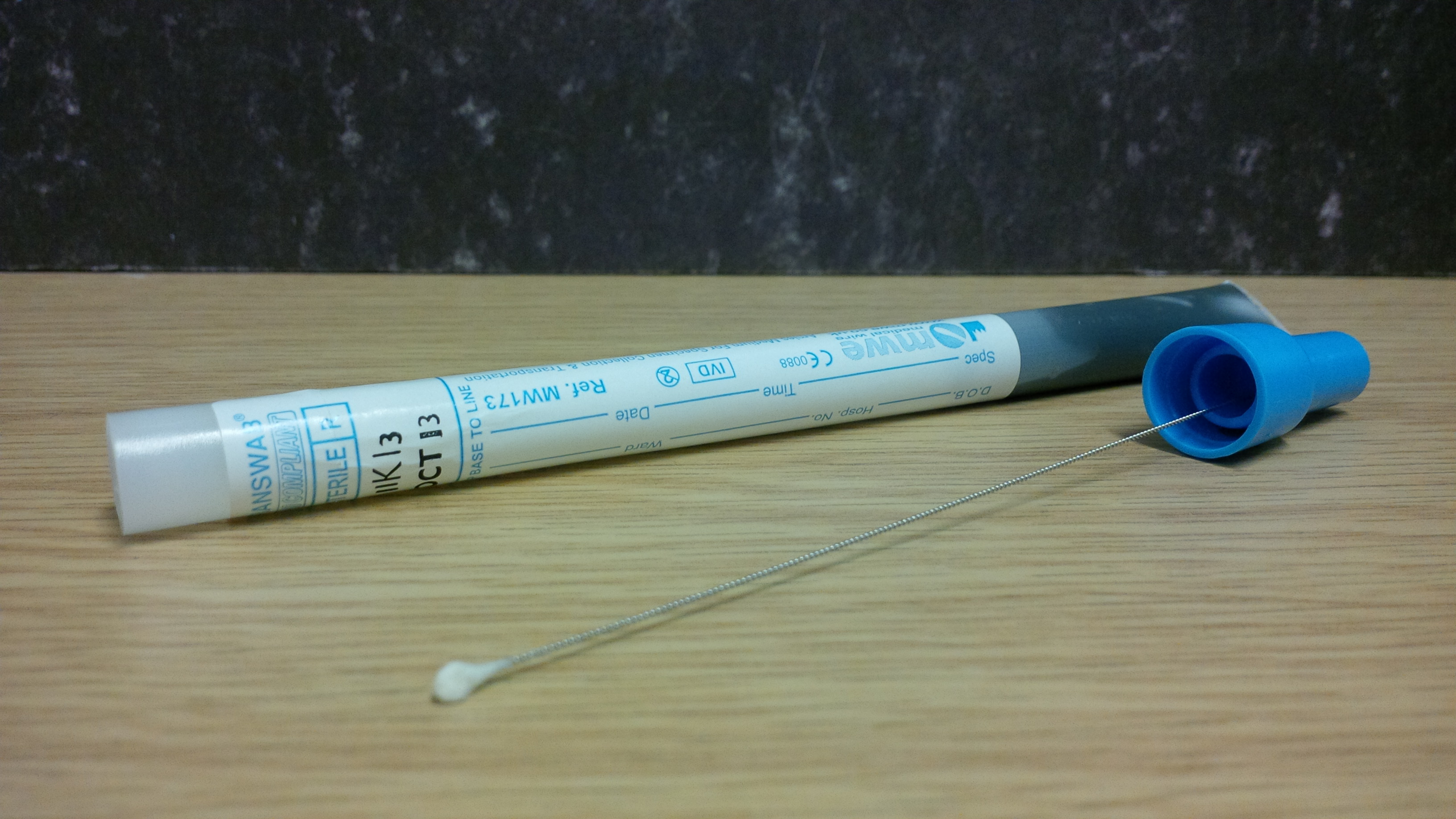
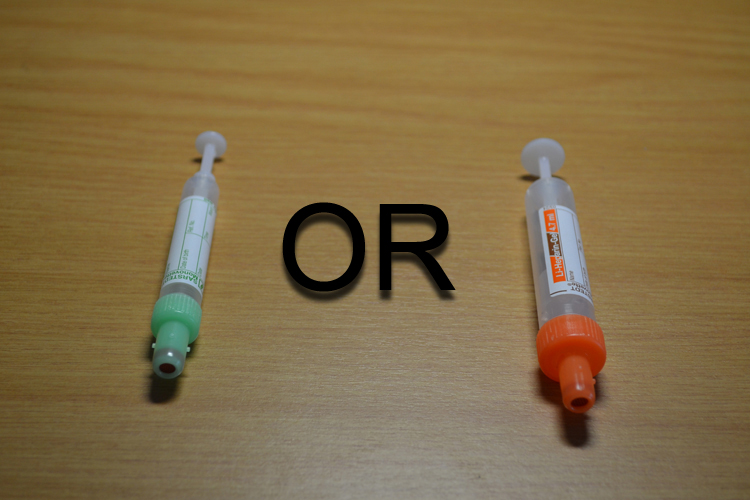
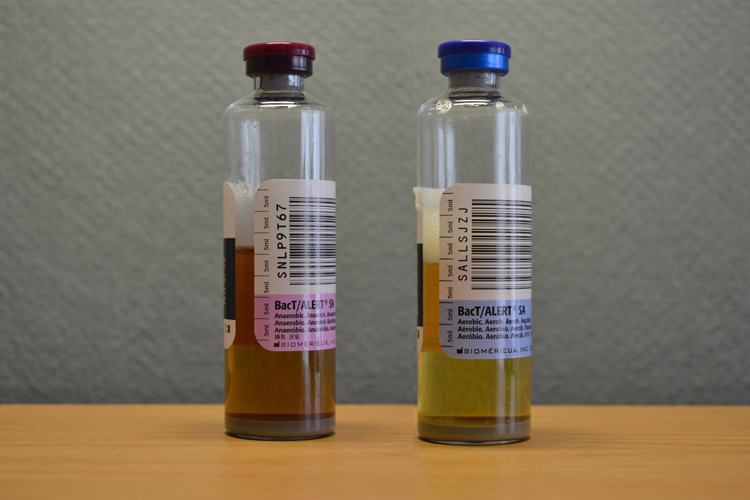
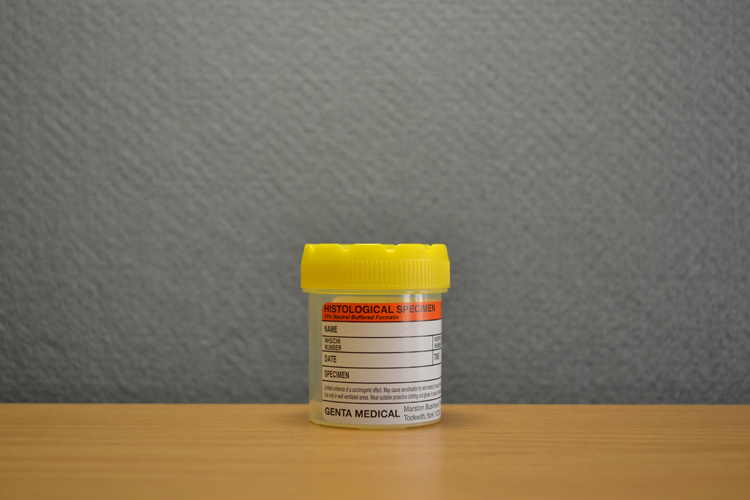
Samples should be collected in to a brown serum tube. If samples are being sent from an external laboratory, separate and send the serum fraction.
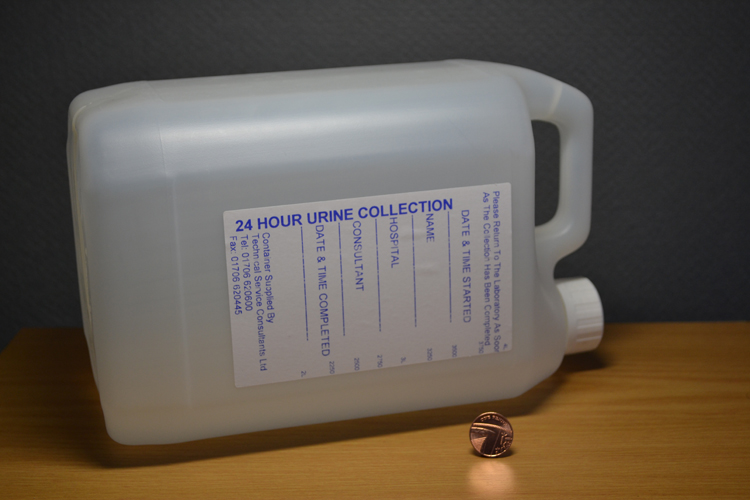
If a patient has experienced an apnoea you should wait at least 24 hours before collecting a sample in order to ensure that there is no drug present in the sample as this can cause erroneous results in the assay.
What do the results mean?
Enzyme activities that are reported as being lower than expected for phenotype could be due to the following factors;
· Birth : 50% level of adults (up to 6 weeks). From 6 wks to 6 yrs a steady rise to levels greater than adults, followed by a fall to adult levels by puberty.
· In pregnancy, levels fall by approx 30%, returning to normal about 6 wks post partum.
· Acute hepatitis & chronic hepatitis
· Cirrhosis and metastases in the liver
· Acute Infections
· Pulmonary embolism
· Muscular dystrophy
· Following surgical procedures
· MI
· Chronic renal disease
· Organic phosphorus insecticides
· Oral Contraceptives – after 3 months of taking a variety of combined OCPs there was a decrease in the mean cholinesterase activity of 20%
· Competitive cholinesterase inhibitors
If any of these conditions exist and are transient, enzyme levels should be checked on recovery.
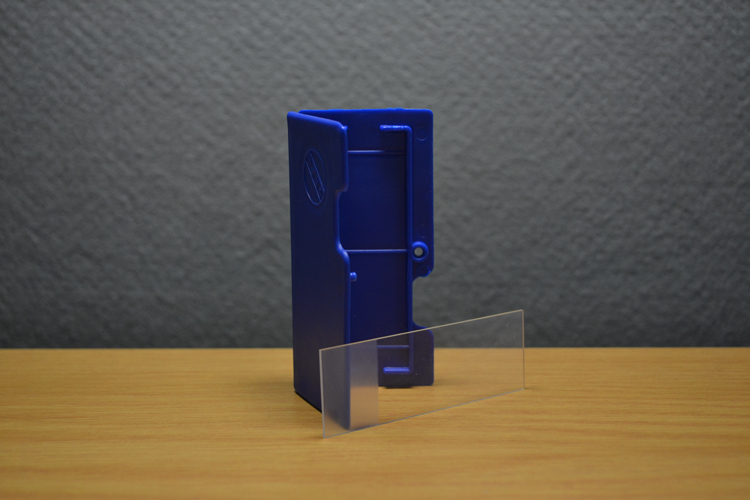
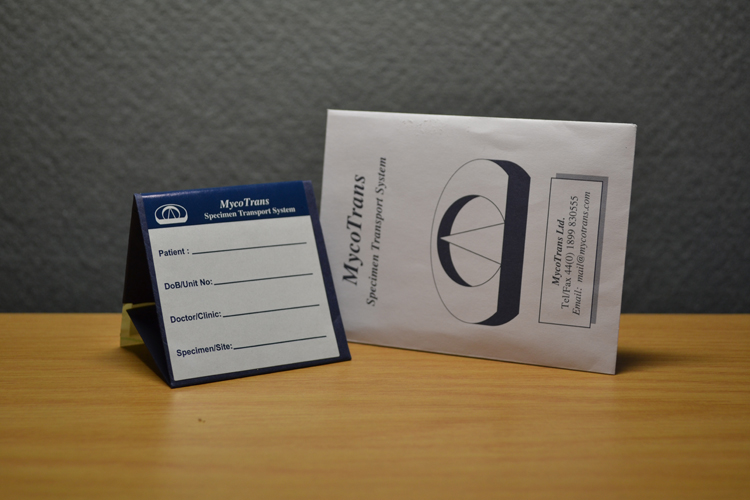
The Butyrylcholinesterase phenotype is determined in an autosomal dominant manner; one allele inherited is from each parent and has an equal effect such that the presence of both alleles together produces an intermediate effect. If hydrolysis in the assay occurs in a ‘normal’ manner, the phenotype of the patient is ‘Usual’ and risk of paralysis is extremely rare. If however hydrolysis is significantly reduced (representing a high risk of muscle paralysis) the phenotype is ‘Atypical’ and paralysis of two or more hours may be experienced. Some patients will have phenotypes that are intermediate between these and will be represented on the report by two different letters, e.g. UA, AK, AJ. The risk associated with each phenotype will be provided on the report and the laboratory will advise on the need for any further family studies. The laboratory will provide a warning card for all patients who are deemed to be at high risk of sensitivity. This should be carried by the patient so that it can be shown to any surgical team in the future to enable the anaesthetist to give a safe muscle relaxant.
What other drugs might be affected?
Cocaine: There are three major routes for the metabolism of cocaine, the most rapid being Butyrylcholinesterase which is responsible for 50% of a given dose. Cholinesterase deficiency may lead to increased plasma concentrations of cocaine in people abusing cocaine and as such they may be more at risk of toxic effects.
Ester local anaesthetics and articaine are best avoided in patients who have a cholinesterase deficiency. This is easily accomplished in dentistry as esters are rarely used as injectables, and primarily used as topicals (benzocaine). Although articaine is an amide, it does have an ester side chain, so it too would be contraindicated. For any dental patient with any level of cholinesterase deficiency one of lidocaine, mepivacaine, or prilocaine may be the best local anaesthetic for dental procedures.
Cholinesterase requesting when organophosphate poisoning is suspected.
Diagnosis of organophosphate poisoning is usually clinical, however the finding of a low cholinesterase activity can be supportive. It should be noted that a low enzyme level alone is not diagnostic, unless the patient has a pre-exposure level for comparison, or if an abnormal phenotype or other causes of a low enzyme activity can be excluded. Any urgent requests should be discussed with the duty biochemist (0131 2426879). Any samples with a low activity should ideally be phenotyped, although this is a manual procedure and results cannot be provided as urgently. ‘Normal’ activity levels do not exclude exposure to organophophates, if that level is significantly lower than the patient’s baseline level.
Organic phosphorus insecticides (eg. Parathion, Sarin, tetraethyl pyrophosphate): 40% reduction of serum activity is seen before the first symptoms are felt, a drop of 80% is required before serious neuromuscular effects become apparent. Near or zero levels require emergency treatment with enzyme re-activators (eg pyridine-2-aldoxime). Levels do not return to normal until 5-6 weeks as new enzyme is synthesized by the liver.